When a “late bloomer” does not bloom
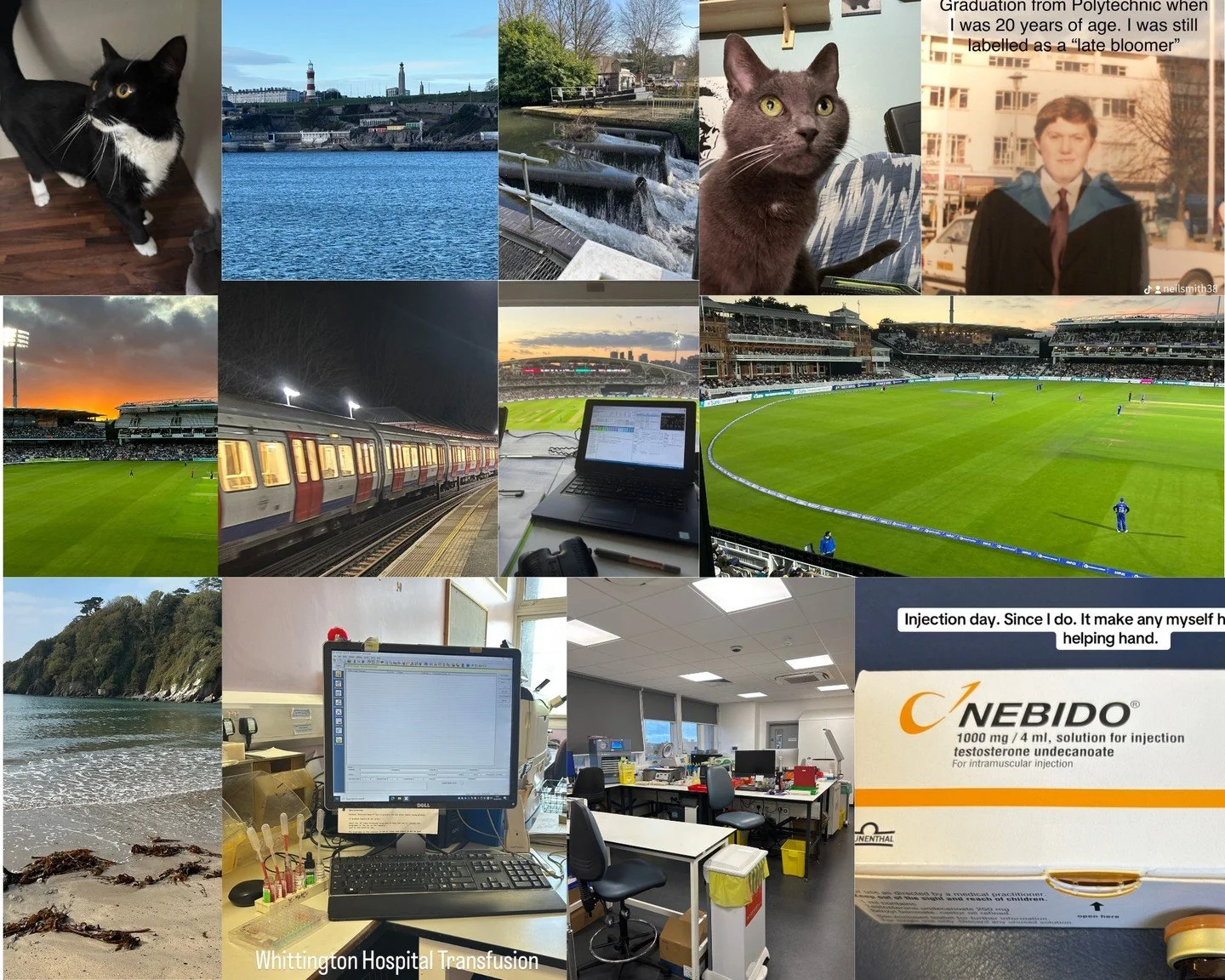
I did not start puberty on time and was labelled as a “late bloomer”.
By the age of 15, I still had not started puberty.
An examination by a school nurse resulted in a trip to the local doctor. He just said I was a “late bloomer” and I should just “wait and see”
No blood tests, no other physical examination.
At the age of 18 I saw two hospital consultants, a urologist and a general medicine consultant but the answer came back the same.
No doctor I spoke to picked up on the fact I also had poor hearing and no sense of smell.
I did not know it at the time but both these symptoms were linked to my lack of puberty.
I went to University to study biomedical sciences. I still had not started puberty.
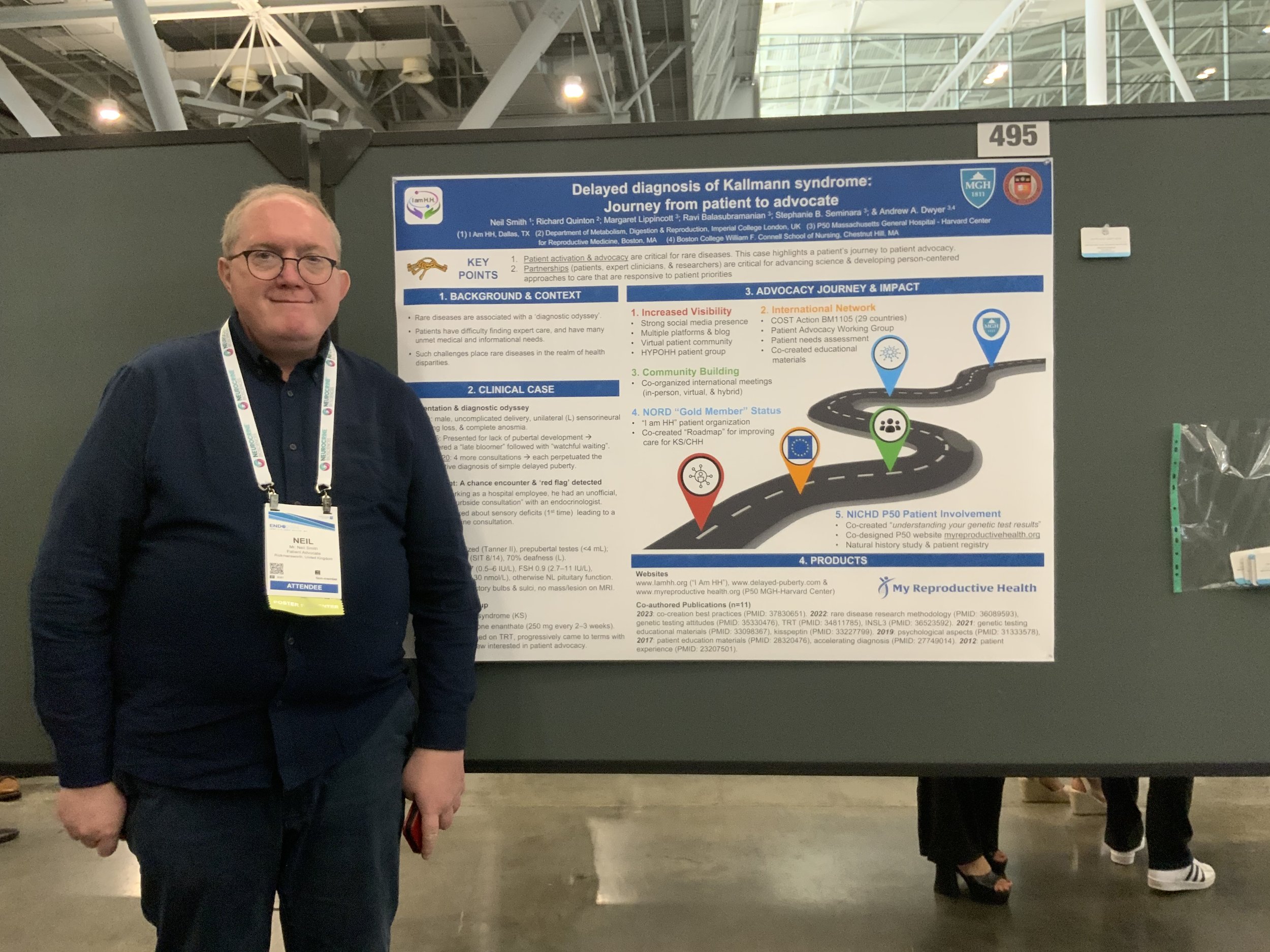
I started work in the my first real job as a Biomedical Scientist at the Royal Free Hospital in London. A chance lunch time meeting with an endocrinologist (Dr Richard Quinton) working there changed everything.
After I first described my symptoms, he asked if I had a sense of smell. That one question led to my diagnosis of Kallmann syndrome.
I have been on testosterone therapy every since. I have to be on some form of hormone replacement. I still did not go through normal puberty but at least got most of the physical changes that should have happened. I would have to take a different form of treatment should I wish to be fertile.
Diagnosis of delayed puberty. - not always a case of “wait and see”.
Some points that were mentioned at the talks I went to at the conference on delayed puberty and Kallmann syndrome / CHH.
About 80% of males who have delayed puberty at the age of 14 will progress to normal puberty with no treatment or a short course of treatment.
30 - 55% of females who have delayed puberty at the age of 13 will progress to normal puberty.
Treatment is not normally required before the age of 13, however treatment need not be with held until a full diagnosis is obtained. Better outcomes both physically and emotionally can be obtained with earlier treatment.
Commencement of puberty (past Tanner stage 2) does not always mean puberty will complete fully in cases other than standard self limiting delayed puberty.
In females treatment with oestrogen only is suggested until maximum uterine growth is obtained (shown by 2 consecutive ultrasound scans). Progesterone should only be added later.
In males with Kallmann syndrome / CHH whose testicle volume is low (2 ml by ultrasound) should not be given hCG on its own when a teenager or young adult as this can reduce the chances of fertility treatment working later in life.
Treatment with testosterone only at any age has no effect (positive or negative) on future fertility chances.
Early use of gonadotropin therapy / fertility treatment in teenagers does not increase the chances of fertility chances working later in life but can reduce the time required to achieve sperm production.
The Kisspeptin challenge test could be a good diagnostic test to distinguish between self limiting delayed puberty and Kallmann syndrome / CHH. It is still only available as a research test but it is hoped that it will be available more widely at some stage.
Inhibin-B is a hormone that is released early in puberty and can be detected during childhood before the age puberty is due. While not always available in all hospital labs, measuring Inhibin-B levels could indicate puberty is starting years before any physical signs can be seen.
Survey for male KS / CHH patients on fertility treatments.
A team of endocrinologists at Imperial College in the UK are planning a large study to look at fertility treatments for male KS / CHH patients in order to establish best practice guidelines.
As part of this study they have created this short survey for any KS / CHH to complete to pass on their experiences and opinions on fertility treatments. They want to know the issues and questions male KS / CHH patients have on fertility treatments.
No medical information or personal information is required, they just want to hear patient views and opinions on fertility treatments to help them plan the full study. All male patients can take the survey, regardless if they have had treatment or not, or where they live.
Talking about Kallmann syndrome to others.
I do not mind talking about my condition to anybody who is willing to listen. I would not go far as to say I enjoy talking about the condition but I do appreciate the chance of trying to raise awareness of the condition.
I do like the "first patient" conversations, where I am the first fellow patient somebody has ever talked to. These conversations can last for hours and often will cover the same questions. I am happy to talk about my experiences with the condition, both positive and negative, if it helps a fellow patient learn more about the condition.
It is the psychological / emotional side of having Kallmann syndrome / CHH which creates the more intense conversations. I have not handled the emotional and physical relationship side of having the condition well. I am happy to talk about my experiences, it might help others not make the same mistakes.
Due to the personal / intimate nature of the condition it is not an easy one to discuss with anybody sometimes, even fellow patients. I tend to be as open as possible, even to the point of over sharing perhaps but I do think it can help some patients to be able to talk other patients who understand the condition.
As with any rare disorder it is perhaps only fellow patients who understand what it is like to have the condition. Puberty is such a natural process normally it can be difficult for others to appreciate what it is like not to go through it correctly or fully.
.
My initial Kallmann syndrome diagnosis.
There is one day in my life I wish I had more memory of, or at least understood the consequences of that day at the time.
The day I got my Kallmann Syndrome diagnosis in 1992.
I studied an endocrinology unit while at University for my biomedical science degreee and had tried to find more information on disorders of puberty, but this was pre internet days and you had to physically find information for yourself in real books.
I started work at a hospital in London as a biomedical scientist, working in a blood transfusion lab. I knew I had an endocrine condition so one day I went up to the endocrine department to find somebody to talk to. No appointment, just one lunch time, knocked on a door.
I wish I could remember the exact details but it involved me telling this endocrine doctor my situation. The first question he asked was "did I have a sense of smell ?".
23 years of age, no doctor had asked me that before. To be fair I perhaps had not thought of telling a doctor either since it was something I rarely thought about.
That doctor was Dr Richard Quinton. At the time senior registrar to Prof Pierre Bouloux. I just happened to start work in the one hospital in the UK that had two KS specialist doctors working there. Dr Quinton had done his MD thesis at Cambridge University on Kallmann syndrome.
This led on to the formal diagnosis and treatment and more importantly perhaps, meeting my first ever fellow patient (that I knew of at least).
I perhaps could not have been at better hospital to get diagnosed for a rare endocrine condition. Getting on to 30 years later I am still in contact with Dr Quinton.
Ovitrelle injection.
Since Pregnyl is no longer available in a lot of places I have had to switch to a different form of hCG injection.
The Ovitrelle pen is designed for female use and at 6,500 IU it is normally too high a dose for single use for males. The dose can be adjusted via the dial “clicks” to get the required dose.
The dose will be set by a health care professional depending on the testosterone level response.
hCG = human chorionic gonadotropin.
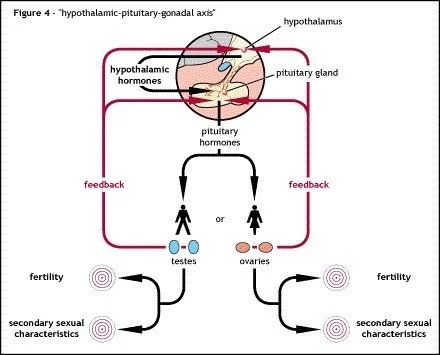
hCG is a natural hormone that mimics the activity of luteinising hormone (LH) which normally makes the testicles produce natural testosterone. LH is one of the two pituitary derived hormones that is missing in Kallmann syndrome / CHH patients.
Types of treatment for Kallmann syndrome / CHH.
Treatment for Kallmann syndrome / CHH can fall into two different types:
Hormone replacement therapy (HRT)
or
Fertility treatment - known as gonadotropin therapy.
Over the years I have been on many forms of HRT and have undertaken fertility treatment as part of clinical trials
Some treatment methods will not be available in every country.
Some treatment methods may work better than others depending on the individual and it may take some discussion with the health care professional to find the method and dose that works best.
How is Kallmann syndrome / CHH diagnosed ?
There is no gold standard single test for Kallmann syndrome / congenital hypogonadotropic hypogonadism (CHH).
Diagnosis is often made by excluding other possible conditions that could affect puberty or fertility
Standard blood tests would include:
Testosterone or oestrogen / progesterone
LH
FSH
Prolactin
SHBG
Vitamin D
Other tests could include:
MRI to examine the size and structure of the pituitary gland and check to see if olfactory bulb is present.
Smell identication test.
Wrist x-ray to determine bone age.
DEXA / DXA bone density scan.
Hearing test.
Neurological exam to check reflexes.
Genetic testing may be undertaken whch can help in some cases, especially if there is a family history of the condition but not all cases of Kallmann syndrome / CHH can be identified through genetics.
What are the major symptoms of Kallmann syndrome ?
The defining symptom of Kallmann syndrome is a lack of sense of smell (anosmia) or a reduced sense of smell.
The condition can also occur with a normal sense of smell when the condition is called hypogonadotropic hypogonadism (HH).
There are other additional symptoms that may or may not occur. Kallmann syndrome or HH show a range of symptoms and patients may not experience any of them or only one them.
Possible additional symptoms:
Hearing loss
Cleft lip / palate
Fused fingers / toes
Missing teeth
Curvature of the back (scoliosis)
Mirror movements of the hands
Missing kidney