6.What happens during normal puberty ?
The physical features of males and females can be divided into two main groups: the primary and the secondary sexual characteristics.
In the majority of cases the primary sexual characteristics are not affected in Kallmann syndrome. and CHH. This is due to the influence of hormones produced by the placenta during pregnancy.
A small majority of boys with Kallmann syndrome are born with un-descended testes, but this is not unique to Kallmann syndrome.
The primary and secondary sexual characteristics are listed in Table 1.
Puberty is not something which happens overnight; it often takes three or four years to complete. It is the transition period during which boys acquire the physical characteristics of adult men and girls those of adult women. Research has shown that generally, girls reach puberty by the age of 14, a year or two earlier than boys.
Take a look at Figure 5.
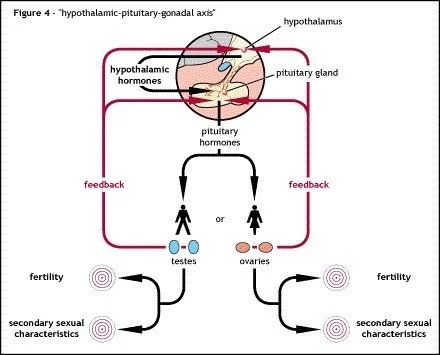
Normally GnRH (gonadotropin releasing hormone) is released by the hypothalamus and delivered to the pituitary gland via a network of capillaries.
GnRH is a hormone which is located in only a very small area of the body and is not normally found in the blood stream. It is not possible to detect the GnRH levels through a blood test.
As its name suggests GnRH causes the release of gonadotropins from the pituitary gland.
The suffix -tropin means "the nourishment of" and so a literal translation of "gonadotropin" is "the nourishment of the gonads". There are two main gonadotropins: LH and FSH, the "Luteinizing Hormone" and "Follicle Stimulating Hormone", respectively.
In some countries, GnRH is also known as LHRH, the "Luteinizing Hormone Releasing Hormone", although this can be a little misleading because it is not only LH, but also FSH which is released by GnRH / LHRH.
Function of the gonadotrophins in men during and after puberty
LH and FSH target different cells with different functions in the testes. In simple terms, LH encourages masculinity and FSH promotes fertility.
In the normal male, LH targets special cells called Leydig cells or interstitial cells and it is here that almost 95% of the main male sex hormone testosterone is made. The remaining 5% of testosterone is manufactured by the adrenal glands, located just above the kidneys.
Testosterone is responsible for the development of the male body's secondary sexual characteristics during puberty (Table 1).
FSH, with a little help from the testosterone produced by the testes, stimulates the production of sperm cells, a process known as spermatogenesis . Sperm cell production can take up to 76 days to be completed from beginning to end.
Function of the gonadotrophins in women during and after puberty
A healthy woman also has levels of the gonadotropins LH and FSH in her blood but her body responds rather differently to these hormones than a man's. Whereas a man has relatively constant levels of LH and FSH, a woman has a regular monthly cycle during which her gonadotropin levels vary from day-to-day. This is called the menstrual cycle and this is illustrated in Figure 6.
In a woman, LH and FSH are both released into the bloodstream in response to the GnRH delivered by the hypothalamus to the pituitary gland. Together with LH and FSH, two other hormones regulate the menstrual cycle.
These hormones are oestrogen and progesterone. In addition, oestrogen encourages the development of the female secondary sexual characteristics (Table 1) and most of it is made by the ovaries, but a little oestrogen is also made by the adrenal glands. Progesterone is responsible for thickening the active layer of the uterus or womb, preparing it for possible pregnancy. The main sources of progesterone are the ovaries, but during pregnancy, the production of progesterone is taken care of by the placenta, an organ attached to the uterus which holds and nourishes the growing embryo. LH and FSH are indirectly responsible for the presence of oestrogen and progesterone in the blood.
For the first few days of the menstrual cycle, a certain amount of bleeding occurs. This is known as menstruation. During menstruation (1), progesterone levels are low. Since progesterone helps to maintain the active layer (endometrium) of the uterus, low levels result in the shedding of much of the endometrium, taking tiny blood vessels which have grown over the previous few weeks with it. At this point, the blood contains medium levels of LH and FSH and only a little oestrogen.
Over the next week or so, oestrogen, LH and FSH begin to increase until about halfway through the menstrual cycle, when ovulation (2) occurs. It is during ovulation that an egg is released from the ovary and slowly travels to the uterus. Only one sperm cell is needed to fertilise the released egg.
Just before ovulation, LH, FSH and oestrogen levels are high but progesterone is still low. Soon after ovulation, hormone levels decrease rapidly except for progesterone, which gradually reaches its peak level on around the 21st day of the menstrual cycle (3) and the endometrium is therefore at its thickest.
If the released egg is not fertilised during this time, the blood begins to "lose" progesterone. When progesterone is at its lowest level (4), the thick endometrium can no longer be supported. It begins to degenerate, menstruation occurs and the menstrual cycle starts again (1).