7. How does having Kallmann syndrome affect puberty ?
Absent or not fully completed puberty is one of the main characteristics of Kallmann syndrome.
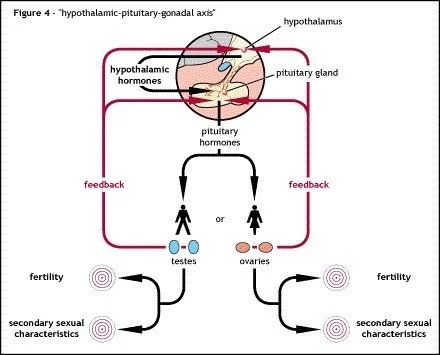
The function of the hypothalamic-pituitary-gonadal axis (described in the answer to Question 5) is interrupted in the case of Kallmann syndrome. Puberty fails to occur and consequently, although the primary sexual characteristics may be intact, the full development of the secondary sexual characteristics are delayed until the patient receives appropriate medical treatment over a number of years which artificially encourages puberty.
Normally the developing baby receives hormones from the mother which help in the development of the primary sexual characteristics. For the most part this is unaffected in Kallmann syndrome. This means that babies born with Kallmann syndrome normally, but not always, show the standard male or female primary sexual characteristics.
With the help of Figure 7, you will see that your hypothalamus is unable to produce and release GnRH. This is because the hypothalamus does not contain enough GnRH cells in order to release enough GnRH to activate the pituitary. Occasionally, especially in females the hypothalamus does have the correct number of GnRH releasing cells but the hypothalamus is unable to release GnRH in the correct manner to enable the pituitary to respond.
Consequently, none of the other hormones needed for pubertal development can be released into your blood to perform their respective tasks. How does all this relate to you ?
The man with Kallmann syndrome
Without GnRH, no LH or FSH can be released from the pituitary. Without LH no testosterone apart from the relatively small amount (about 5%) from your adrenal glands is produced. Without FSH, growth, development and maturation of the sperm cells are unable to occur, so the testes remain virtually at their pre-pubertal size. Even though semen will be produced during ejaculation there will be no sperm cells present meaning the vast majority of men with Kallmann syndrome will be infertile and will remain so without specialised treatment.
Secondary sexual characteristics are virtually non-existent or only partially present. Typically, untreated men with Kallmann syndrome have high-pitched voices, little redistributed muscle tissue and testes the size of those of pre-pubertal boys (normally less than 4ml in size). A small percentage of men with Kallmann syndrome are also born with undescended testes and a small penis, known as microphallus, however these symptoms are not unique to Kallmann syndrome.
It is possible to induce puberty artificially through hormonal replacement therapy, normally with testosterone but just like normal puberty, artificial inducement may take several years. If testosterone is used it will not be a totally normal puberty as there will be no testicular enlargement. If treatment is started at the appropriate age all the other secondary sexual characteristics should develop as normal.
However, even once the secondary sexual characteristics have been restored treatment normally will have to continue on a permanent basis.
Fertility treatments are also available which can be successful for the majority of men with Kallmann syndrome, however there are a number of factors doctors will have to take into account before deciding on starting treatment.
The woman with Kallmann syndrome.
An untreated woman with Kallmann syndrome will also not develop the normal secondary sexual characteristics and normally be infertile. The hips will not widen, there will be little breast development and space pubic hair growth. Internally the uterus will remain small in size and the ovaries will not be functional.
Unlike men where there is no testicular growth so there are no sperm cells in women with Kallmann syndrome the ovaries do normally contain the normal number of immature eggs. However without the influence of LH and FSH from the pituitary the eggs are not able to mature and there is very little production of oestrogen and progesterone.
In the answer to Question 6 the normal menstrual cycle was discussed. Since both LH and FSH help to regulate the menstrual cycle, their absence results in the lack of menstruation. This is called primary amenorrhea. There are many different causes of amenorrhea in women, both medical and environmental and it is sometimes the case that Kallmann syndrome is quite low down the list of possible causes and can be easily overlooked.
Figure 8 illustrates why amenorrhea occurs in women with Kallmann syndrome. Amenorrhoea occurs because there is no LH or FSH produced by pituitary and therefore the ovaries cannot manufacture the required amounts of oestrogen and progesterone.
As with males a very small amount of oestrogen is produced by the adrenal glands but this normal not sufficient for the normal working of the body. With these extremely low hormone levels (progesterone in particular), the uterus cannot work properly because its active layer (endometrium) fails to thicken.
The lack of menstruation can be corrected with the use of hormone replacement therapy. Several different types of therapy are available on the NHS and in almost all cases, the normal menstrual cycle can be simulated as closely as possible for as long as treatment is given. If treatment is stopped though, the menstrual cycle can no longer be maintained and amenorrhoea eventually returns. Hormone replacement therapy is discussed in more detail later in the answers to Questions 19 and 24.
Initial treatment for younger women with Kallmann syndrome is often with oestrogen only to allow the full development of the secondary sexual characteristics. Only later is progesterone added to allow for the healthy development of the uterine lining.
Sometimes women are prescribed the combined oral contraceptive pill which contains both oestrogen and progesterone. A one week gap every month or three months allows the uterine lining to be shed to mimic a menstrual bleed.