When a “late bloomer” does not bloom
I did not start puberty on time and was labelled as a “late bloomer”.
By the age of 15, I still had not started puberty.
An examination by a school nurse resulted in a trip to the local doctor. He just said I was a “late bloomer” and I should just “wait and see”
No blood tests, no other physical examination.
At the age of 18 I saw two hospital consultants, a urologist and a general medicine consultant but the answer came back the same.
No doctor I spoke to picked up on the fact I also had poor hearing and no sense of smell.
I did not know it at the time but both these symptoms were linked to my lack of puberty.
I went to University to study biomedical sciences. I still had not started puberty.
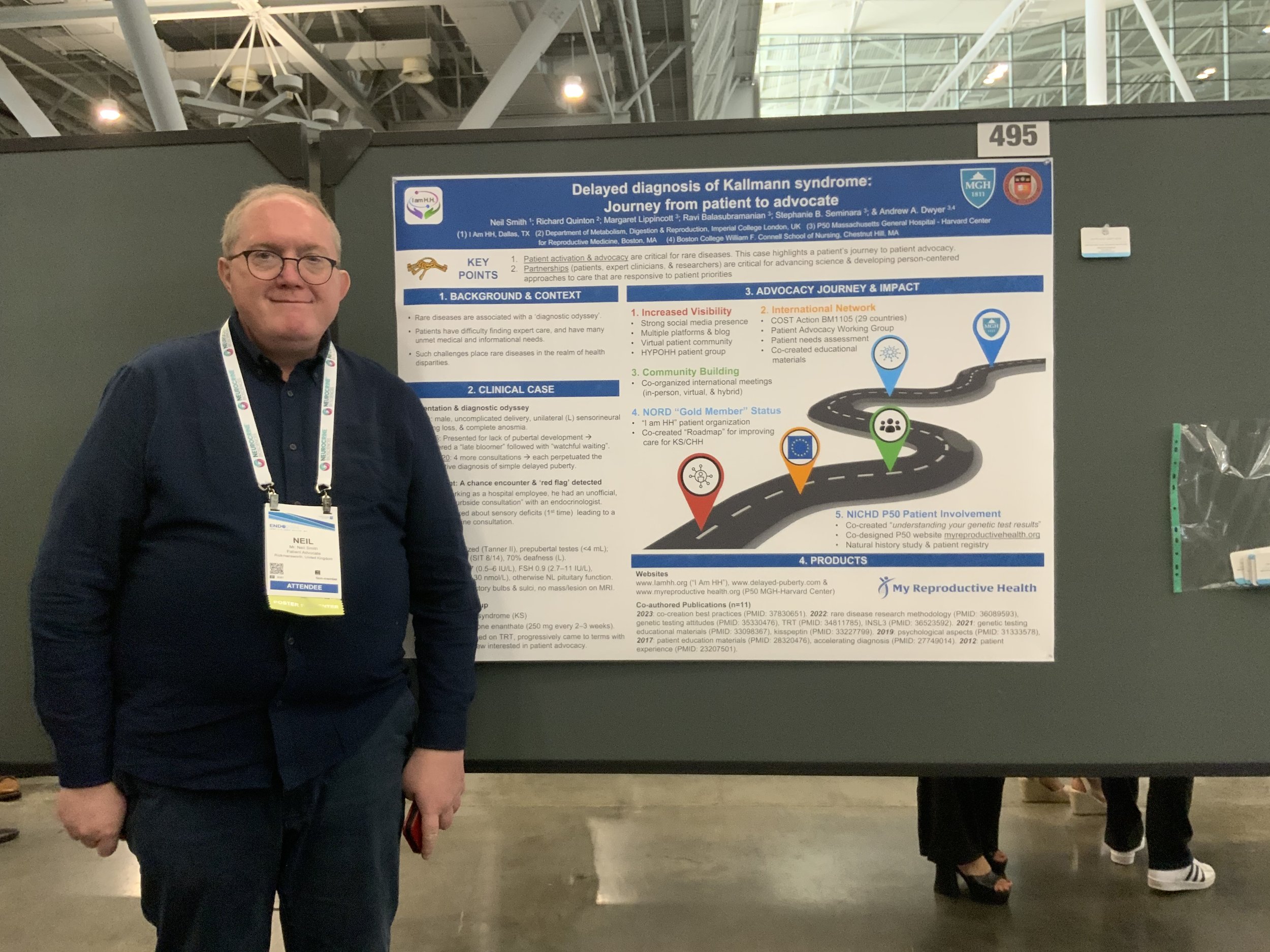
I started work in the my first real job as a Biomedical Scientist at the Royal Free Hospital in London. A chance lunch time meeting with an endocrinologist (Dr Richard Quinton) working there changed everything.
After I first described my symptoms, he asked if I had a sense of smell. That one question led to my diagnosis of Kallmann syndrome.
I have been on testosterone therapy every since. I have to be on some form of hormone replacement. I still did not go through normal puberty but at least got most of the physical changes that should have happened. I would have to take a different form of treatment should I wish to be fertile.
Diagnosis of delayed puberty. - not always a case of “wait and see”.
Some points that were mentioned at the talks I went to at the conference on delayed puberty and Kallmann syndrome / CHH.
About 80% of males who have delayed puberty at the age of 14 will progress to normal puberty with no treatment or a short course of treatment.
30 - 55% of females who have delayed puberty at the age of 13 will progress to normal puberty.
Treatment is not normally required before the age of 13, however treatment need not be with held until a full diagnosis is obtained. Better outcomes both physically and emotionally can be obtained with earlier treatment.
Commencement of puberty (past Tanner stage 2) does not always mean puberty will complete fully in cases other than standard self limiting delayed puberty.
In females treatment with oestrogen only is suggested until maximum uterine growth is obtained (shown by 2 consecutive ultrasound scans). Progesterone should only be added later.
In males with Kallmann syndrome / CHH whose testicle volume is low (2 ml by ultrasound) should not be given hCG on its own when a teenager or young adult as this can reduce the chances of fertility treatment working later in life.
Treatment with testosterone only at any age has no effect (positive or negative) on future fertility chances.
Early use of gonadotropin therapy / fertility treatment in teenagers does not increase the chances of fertility chances working later in life but can reduce the time required to achieve sperm production.
The Kisspeptin challenge test could be a good diagnostic test to distinguish between self limiting delayed puberty and Kallmann syndrome / CHH. It is still only available as a research test but it is hoped that it will be available more widely at some stage.
Inhibin-B is a hormone that is released early in puberty and can be detected during childhood before the age puberty is due. While not always available in all hospital labs, measuring Inhibin-B levels could indicate puberty is starting years before any physical signs can be seen.
Having Kallmann syndrome is not the same as being a "late bloomer"
Being a late bloomer can be difficult enough for people, there can be a feeling of being left behind both emotional and physically.
Patients with Kallmann syndrome / hypogonadotropic hypogonadism can sometimes be labelled as “late bloomers” even when other symptoms are present.
This can delay diagnosis and treatment which can affect patients both physically and emotionally.
Kallmann syndrome - AI generated text.
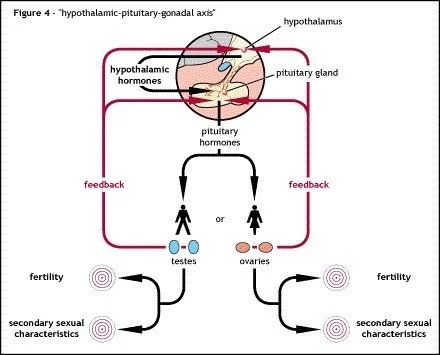
Kallmann syndrome is a rare genetic disorder that is characterized by delayed or incomplete puberty along with an impaired sense of smell. This condition is caused by a deficiency in the production of certain hormones that are crucial for both puberty and the sense of smell. Individuals with Kallmann syndrome may also experience infertility due to these hormonal imbalances. Treatment typically involves hormone replacement therapy to induce puberty and address any related symptoms. Early diagnosis and appropriate management are essential in helping individuals with Kallmann syndrome lead healthy and fulfilling lives.
A good attempt by AI but some points I would like to add as a patient with Kallmann syndrome.
Hormones do not affect the sense of smell. The lack of sense of smell comes from the nerves controlling the sense of smell not being in the correct location within the olfactory bulb (“smell centre”) of the brain.
Patients with Kallmann syndrome are most likely to be infertile due to lack of gonadotropins (FSH / LH) produced by the pituitary gland. A small minority of patients with partial or incomplete Kallmann syndrome will have a low level of sperm / egg production & fertility.
Patients with Kallmann syndrome do not experience normal puberty even when on treatment. Standard hormone replacement therapy (testosterone or progesterone / oestrogen) will produce most of the secondary physical characteristics normally seen at puberty but will not induce fertility in either male or female patients.
Talking about Kallmann syndrome to others.
I do not mind talking about my condition to anybody who is willing to listen. I would not go far as to say I enjoy talking about the condition but I do appreciate the chance of trying to raise awareness of the condition.
I do like the "first patient" conversations, where I am the first fellow patient somebody has ever talked to. These conversations can last for hours and often will cover the same questions. I am happy to talk about my experiences with the condition, both positive and negative, if it helps a fellow patient learn more about the condition.
It is the psychological / emotional side of having Kallmann syndrome / CHH which creates the more intense conversations. I have not handled the emotional and physical relationship side of having the condition well. I am happy to talk about my experiences, it might help others not make the same mistakes.
Due to the personal / intimate nature of the condition it is not an easy one to discuss with anybody sometimes, even fellow patients. I tend to be as open as possible, even to the point of over sharing perhaps but I do think it can help some patients to be able to talk other patients who understand the condition.
As with any rare disorder it is perhaps only fellow patients who understand what it is like to have the condition. Puberty is such a natural process normally it can be difficult for others to appreciate what it is like not to go through it correctly or fully.
.